The Science Behind How Aphasia Affects Your Brain
It came as a shock when Bruce Willis' family recently announced that he would be permanently retiring from acting. Per Variety, the family cited Willis' recent health problems and diagnosis of aphasia — a neurological disorder that affects the speech centers of the brain — as the reason for his departure from film and TV. This prompted many to ask, "What is aphasia, exactly?"
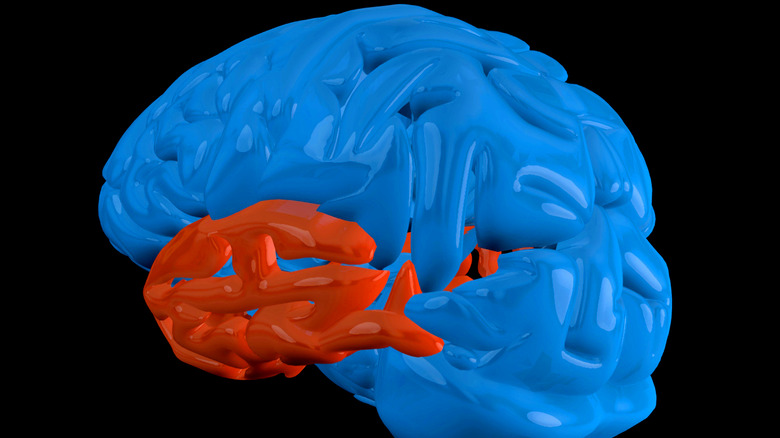
As the National Institute on Deafness and other Communicative Disorders describes, aphasia refers to a group of disorders resulting from problems with the language-processing parts of the brain, specifically Broca's area and Wernicke's area. Broca's area is responsible for listening comprehension, and Wernicke's area for language production. People with damage to these areas of the brain can still listen and speak, but their language integration and grammar production, aka "semantics," is stymied or garbled.
If Broca's area is damaged, then a person can understand spoken language just fine, but can't generate vocabulary or proper grammar. They might say "Big cheese get" instead of "I would like to buy a large cheese pizza." People with damage to Wernicke's area have the opposite problem. Their understanding of spoken language is muddled, and as a result, their sentences tend to come out in long, unbroken strands like, "You know I got that whale wheedled when it hit the one that you wanted to hear about tomorrow outside." People with damage to both areas have "global aphasia."
A long path to a recent diagnosis
It's easy to see how a disorder like aphasia can be extremely frustrating to those who have it, and those around them. People with aphasia understand what they mean, within their own minds, but can't communicate it properly. If you've ever struggled to find the right word to finish a sentence, then you can glean what it feels like to have Broca's (non-fluent) aphasia. And if you've ever rambled while wrestling to get your point across, and had no one understand you, then you can glean what it feels like to have Wernicke's (fluent) aphasia.
Aphasia wasn't properly understood until recently, especially after the advent of CT and MRI medical imaging technology in the 1970s, as Science Direct cites, via the Handbook of Clinical Neurology. After all, if a doctor can't properly communicate with a patient, it's hard to diagnose them. Patients with aphasia typically rely on family members and loved ones to communicate on their behalf. It was only due to postmortem studies of patients in the 19th century that researchers began to have an idea of not only aphasia's causes, but the anatomical roots of language processing in the brain.
In 1861, French researcher Paul Broca, after whom Broca's area is named, first identified the connection between specific, local brain damage and an inability to properly process language. He did so, as the National Aphasia Association says, after caring for a patient who couldn't say anything besides "tan."
Strokes and other damage to the brain
As you could imagine, aphasia is a devastating diagnosis to receive, one often compounded by the loss of the ability to hold down a job, relationships strained to the breaking point because of extreme communication difficulties, and resultant diagnoses of other illness like clinical depression.
As the National Institute on Deafness and other Communicative Disorders relates, aphasia can result from any number of causes, particularly strokes that cause blood to stop flowing throughout the brain. The National Aphasia Association states that approximately 25% to 40% of stroke survivors develop aphasia. Other causes include tumors, infections, neurological disorders like Alzheimer's, and physical injury caused by anything ranging from gunshot wounds to blunt force trauma from a car accident. No matter the cause, if language processing centers like Broca's area or Wernicke's area are affected, then aphasia of any type and severity may develop. It's important to remember that there isn't only one kind of aphasia, but many different types resulting from similar causes. It all depends on case-by-case anatomical details.
Because of the influence of age-related, degenerative neurological disorders on the prevalence of aphasia, aphasia is usually more common in older people. (Willis recently turned 67, per Biography.) Besides that, there's no one group of people more susceptible to the development of aphasia than another. At present, aphasia is more common in the U.S. than Parkinson's Disease, cerebral palsy, or muscular dystrophy. Nearly 2 million people suffer from aphasia, and every year about 180,000 more people receive the diagnosis.
The brain's language loop revealed
Understanding aphasia requires an understanding of the brain's different centers, or loci, each of which processes a different action. Even though the right hemisphere of the brain is responsible for the left side of the body, and vice-versa, the division of responsibility between halves isn't strictly separated for something as complex as language processing. It's asymmetrical, including the brain's "language loop." In right-handed people, about 90% of the language loop's functionality is located in the left hemisphere. In left-handed people, responsibility is more shared between hemispheres, with 70% of the language loop being localized in the left hemisphere, as McGill University explains.
These are the kinds of discoveries that went hand-in-hand with research into aphasia, particularly thanks to French neuroscientist Paul Broca in 1861, and then German neuroscientist Carl Wernicke about a decade later. Broca discovered that damage to the left, posterior (bottom-ish) frontal lobe of the brain led to difficulties with language output. Wernicke discovered that damage to the left, posterior temporal lobe (the side of the brain) led to problems with language input. Together, these areas — Broca's area and Wernicke's area, respectively — form the ends of the brain's language loop, which is connected by a bundle of nerves called the arcuate fasciculus that runs along a fissure in the brain called the lateral sulcus. The worst-case diagnoses of aphasia involve the complete obliteration of this language loop, and an inability to speak whatsoever, as the National Aphasia Association illustrates.
A wide array of diagnostic tests and tools
As you could imagine, aphasia remained an utter mystery, and utterly misdiagnosed, in the centuries leading up to modern neuroscience. Doctors use an array of testing methods and medical imaging technology to check for aphasia, as John Hopkins University explains. This allows for a full and complete portrait of the human brain, and any potential injuries, without having to slice open someone's skull.
If a patient exhibits potential symptoms of aphasia, especially after suffering one or more of its typical causes, doctors turn to aphasia assessments as a first line of defense. These formal, clinically designed tools check things like speech patterns, prosody (rhythm and intonation), naming of objects, repetition, language comprehension, reading and writing, and so on. Lingraphica, an ordering site for these kinds of tools, explains how they work in detail. The Mississippi Aphasia Screening Test (MAST), for instance, is a quick 5- to 15-minute oral exam, while the Boston Diagnostic Aphasia Evaluation-3rd Edition (BDAE-3) is a more thorough, involved assessment that checks all aspects of a person's language functions.
On the hi-tech side of diagnoses, we've got CT scans, MRIs, and PET scans. CT scans (computed tomography) use x-rays to take detailed pictures of bone, muscle, tissue, and organs. MRIs (magnetic resonance imaging) produce detailed pictures using radio waves and magnets, while PET scans (positron emission tomography) produce 3D images of metabolic flow using a radioactive drug ingested by patients.
Treatment and therapy for patients and loved ones
Sometimes, as the National Aphasia Association says, aphasia is a temporary condition that plays out as the body heals from an injury. If symptoms persist for more than two or three months, though, especially after a stroke, a complete recovery is unlikely. At that point, there's little in the way of a cure for aphasia. However, as the National Institute on Deafness and other Communicative Disorders says, speech-language therapy can help a person with aphasia learn about their condition and live a full life. Such therapy can be one-on-one or group-based, and involve pictures, gestures, teaching communication techniques, the use of electronic devices, and more. Speech-generating apps are also available to aid in day-to-day conversation. Besides such direct therapy, it's critical for people with aphasia to feel connected to others through support groups and social clubs.
Because loved ones are essential to the recovery and continued support of someone suffering from aphasia, much of the treatment for the disorder revolves around teaching them how to cope, as well. Simple advice like simplifying language, or not correcting the speech of someone who has aphasia, can go a long way to making home life as natural and happy as possible.
Thanks to cutting edge therapy techniques, those with aphasia face a brighter future than before. Transcranial direct current stimulation (tDCS), for instance, directly stimulates the brain's language loop, and may help re-wire a person's ability to speak.