Most Dangerous Surgeries You Can Have
Having surgery can be a frightening experience, no matter how minor the procedure is. Not knowing what will happen during the surgery and post-surgical recovery can be challenging. Also, you may encounter complications, such as bleeding, infection, blood clots, a pulmonary embolism, or an allergic reaction to anesthesia, according to John Hopkins Medicine. This is in addition to common post-surgery issues, such as nausea, pain, and sleeplessness. And depending on the procedure, it can take weeks or months before you're back to normal.
While all surgeries have an inherent risk to them, some are more dangerous than others, particularly if they're not planned in advance. According to a 2016 study published by JAMA Surgery, there are seven emergency procedures in particular that make up 80% of all deaths and complications, including partial colon removal, appendix removal, and ulcer surgery. And, every year, approximately 3 million patients undergo emergency surgery. Over the study's four-year period, the mortality rate for emergency surgery was 1.2%, and the complication rate was 15%.
There are also several other types of surgery that are not emergency in nature but are still quite dangerous due to their complications, including gastric bypass, spinal surgery, and coronary revascularization. Here are the most dangerous surgeries you can have.
Colectomy (Partial Colon Removal)
A colectomy involves the removal of all or part of the colon, also known as the large intestine. This is the long, tube-like organ that makes up part of your digestive tract, according to the Mayo Clinic. Patients need a colectomy for conditions such as uncontrolled bleeding, a bowel obstruction, colon cancer, Crohn's disease, ulcerative colitis, and diverticulitis. Some have a colectomy if they are at high risk for colon cancer, which can be deadly depending on when it's diagnosed and treated.
Patient Alvin Alexander wrote on his blog that he has had seven surgeries over his lifetime, and the colectomy was the most difficult: "I still have to be very careful about what I eat, and I get pain in the lower abdomen both from eating and from weird things, like turning sideways to reach for something. I can imagine that there are much worse surgeries, but this one is difficult."
In addition to the colectomy, many patients also need other surgical procedures that reattach the areas of the digestive system in order to let waste evacuate from the body. This surgery "carries a risk of serious complications." This includes infection, bleeding, deep vein thrombosis (blood clots in the legs), and pulmonary embolism (blood clots in the lungs). Other complications include damage to nearby organs, such as the bladder and small intestines. In addition, you could experience tears in the sutures that are used to reconnect the sections of the digestive system.
Small bowel resection
A small bowel resection surgically removes a diseased portion of your small intestines. It is commonly used to treat Crohn's disease, according to Stamford Health Care. What makes this surgery a bit complicated is that if it's performed too early, more bowel tissue may be removed than is necessary. If it's performed too late, like during an emergency procedure, the complications can be more severe. Small bowel resections are also performed to treat inflammatory bowel disease, Meckel's diverticulum, a blockage in the intestines, GI cancer, noncancerous tumors, and injuries to the small intestine.
If you have a small bowel resection, you may have to cope with the following complications: intestinal bleeding, frequent diarrhea, and an incision tearing open. In addition, you may experience an incisional hernia in which the intestine pushes through the incision and into your stomach. Also, pus may build up in the small bowel, which could necessitate drainage. Scar tissue can cause intestinal blockages, or you may wind up with short bowel syndrome, which prevents your body from absorbing enough nutrients, according to the Mayo Clinic.
Recovery also takes time. One patient wrote on her blog, A Healthy Happy Glow, that four days after the surgery she felt "dizzy, light-headed, nauseous and tired," and she wasn't released from the hospital until about one week after the procedure.
Cholecystectomy (Gallbladder Removal)
The gallbladder is the small organ located on the right side of the stomach that stores bile, which is produced by the liver and reduces the fat from food. Individuals usually have gallbladder surgery to remove gallstones, which are hardened deposits made from bile, according to Everyday Health. This procedure is relatively common, but that doesn't mean it isn't dangerous, particularly if it's performed in an emergency situation. Following surgery, it can be difficult to digest certain types of foods, particularly those that are high in fat and high in fiber content. This can cause abdominal pain, bloating, gas, and diarrhea. However, these symptoms are normal and can be treated with diet.
Unfortunately, there are some dangerous complications that can occur. It's possible to experience bile leakage into the abdomen if the clips used to seal the tube that connects the gallbladder to the main bile duct fails. This can require draining or even an additional operation to drain the bile and clean the abdomen. Other complications include bile duct injury or damage to surrounding blood vessels, the liver, or the intestines. Some patients also experience blood clots in the legs (deep vein thrombosis) or lungs (pulmonary embolism). Infection, bleeding, scars, numbness, and a hernia may also occur.
Patient John Gilstrap wrote of his cholecystectomy experience: "During the removal procedure, the surgeon discovered impacted calculi in my common bile duct, prompting a second emergency procedure (an ERCP — endoscopic retrograde cholangeopancreatography) the following day."
Antrectomy or Pyloroplasty (Peptic ulcer surgery)
You may require peptic ulcer surgery if you have an ulcer that bleeds excessively, you experience agonizing stomach pain, your ulcer is perforated and causing peritonitis, or contents within the stomach are obstructed. The surgery involves several areas: the esophagus, stomach, duodenum, jejunum, and vagus nerves, according to DoveMed. During the procedure, the surgeon may cut the vagus nerve, remove the antrum (the lower portion of the stomach), or enlarge the area between the stomach and the duodenum (part of the small intestine).
During the surgical procedure, complications can include excessive bleeding, infection, and anesthetic issues. In addition, there could be accidental damage to the large blood vessels and nearby nerves in the neck, lungs, thoracic duct, and laryngeal nerve. Post-op complications can also include excessive bleeding and infection, as well as an incisional hernia, recurring peptic ulcers, malnutrition, and extreme diarrhea. In addition, a patient may feel uneasy, uncomfortable and other symptoms after eating certain types of food. Other post-op symptoms can include nausea, vomiting, constipation, rectal bleeding, muscle aches, headache, dizziness, and more.
If left untreated, peptic ulcer perforation, can result in death, according to the National Library of Medicine. In addition, a delay in a correct diagnosis boosts mortality rates. So, the aforementioned complications may be worth the risk.
Abdominal adhesiolysis (removal of abdominal scar tissue)
Surgeries can cause abdominal adhesions, which are lumps of scar tissue in your stomach. You can also get these adhesions from a trauma, infection, or inflammatory condition. These adhesions can form on organs and even cause these organs to stick together, according to Healthline, which can lead to chronic pain or digestive issues. These adhesions can also block the intestines and cause a bowel obstruction, female reproductive problems, or painful intercourse.
The way to remove these adhesions is with a surgical procedure known as abdominal adhesiolysis. Since the scar tissue doesn't appear on imaging tests, doctors usually don't notice them unless they are doing another type of procedure. People with Crohn's disease, endometriosis, pelvic inflammatory disease, peritonitis, and diverticular disease may experience this type of scar tissue. While the surgery is not very invasive, complications can include organ damage, bleeding, infections, a hernia, and even a worsening of the adhesions. It's pretty bad to have surgery to remove adhesions only for the adhesions to get worse afterwards.
A woman named Lisa wrote on Fight Like a Girl that a pelvic exam "showed so many lesions/scar tissue from past C-sections that the scar tissue was strangling my organs and cutting off blood flow, which created a small bowel obstruction." She had surgery and added that she may spend the rest of her life having adhesions removed because they can grow back.
Appendectomy (appendix removal)
The appendix is a small pouch connected to the large intestine on the lower right area of the stomach. If the appendix gets infected, it turns into appendicitis, and it requires an appendectomy, which is often performed during an emergency. If not treated immediately, the appendix can burst, according to Johns Hopkins Medicine. When it comes to emergency surgery, the mortality rate is 5.1 per 1,000 people, according to Medical News Today. Patients usually undergo an open appendectomy in which the surgeon cuts a two-to-four-inch incision on the abdomen and removes the appendix. However, a less invasive laparoscopic appendectomy may also be performed, which uses smaller incisions and a camera to remove the appendix.
Complications of either an open or laparoscopic appendectomy include bleeding, infection in the wound site, and infection, redness, and swelling in the belly that can occur if the appendix bursts during the procedure. Also, it can cause blocked bowels and injury to surrounding organs. Post-op patients are urged to call their doctor for a number of symptoms, including fever or chills, issues around the incision site, abdominal pain, trouble breathing, loss of appetite or vomiting, and continuous problems with bowel movements or diarrhea.
Laparotomy (abdominal surgery)
Abdominal surgery may be performed to remove an appendix or repair a hernia. However, sometimes the causes of abdominal pain and other issues are unclear, which requires an exploratory laparotomy to identify the problem, according to Healthline. This type of surgery is often performed if serious or long-term abdominal problems have yet to be solved or major abdominal trauma has occurred. It's used to examine such things as blood vessels, the small or large intestine, the pancreas, liver, the lymph nodes, the spleen, and more. A laparotomy is not as common as it used to be due to advances in technology, but it can still occur in emergency situations or when diagnostic tests can't explain what the issue is.
Complications of the surgery can include bleeding, infection, an incision that doesn't heal well, injury to the bowels or other organs, and an incisional hernia. Serious complications may be accompanied by a fever, increasing pain, incision infection, chest pain, shortness of breath, a persistent cough, nausea, and more.
A study of 4,346 patients who had emergency abdominal surgery found that nearly one in five patients died after an emergency laparotomy, and "the overall death rate within 24 hours of surgery was 21%."
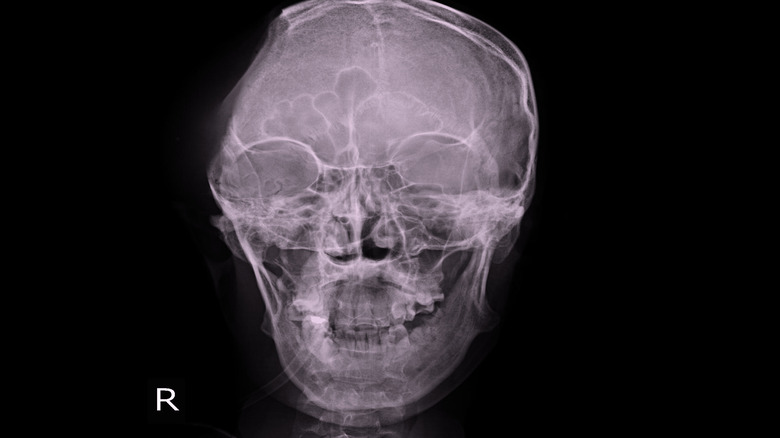
Craniectomy
A craniectomy is typically performed during an emergency in order to save a patient's life. It involves removing part of the skull to relieve pressure, brain swelling, and hemorrhaging. It's commonly performed following a traumatic brain injury, stroke, or if there are blood clots or blockage in the brain arteries, according to Healthline. It's also used to treat a cerebral edema or intracranial hematoma. Patients who have intracranial pressure, intracranial hypertension, or heavy bleeding and do not have a craniectomy can experience pressure or bleeding that can compress the brain and push it towards the brain stem, which can cause brain damage or even death.
According to Medicine, "Treatment of severe traumatic brain injury (TBI) is challenging and often associated with high mortality and morbidity. The mortality rate can be as high as 60% to 84.6% in TBI cases with brain herniation."
As you would expect, there are some major complications that can occur following this type of invasive surgery. This includes permanent brain damage, pooling or infected fluid in the brain, and meningitis (brain inflammation). Patients can also experience bleeding between the brain and scalp, a brain or spine infection, the loss of the ability to speak, or partial or full-body paralysis. Even worse, patients can wind up in a coma, a persistent vegetative state, or experience brain death. While these complications can be terrible, a craniectomy is a life-saving procedure for many people who have experienced a traumatic injury or stroke, so it's worth the risks in many situations.
Separation of Conjoined Twins
Conjoined twins are fused together in utero and remain that way after they are born. The odds of a conjoined twin birth are one per 50,000 to 200,000, according to the National Center for Biotechnology Information. Around 60% of these twins are stillborn. The condition is underreported around the world, so it's unclear how many conjoined twins are actually born each year. The most common type of conjoined twins are joined at the thorax and abdomen. They can also be joined at the sacrum and perineum, vertebral column, lower abdomen and pelvis, and head to umbilicus. In addition, they may be joined at just the thorax, abdomen, or head.
How the twins are fused together indicates whether they can be separated. Generally, 25% of these children live long enough to undergo surgery. Those who share vital organs typically can't be separated as it would cause one or both of them to die. Should parents decide to separate their conjoined twins, complications can include organ failure, skin defects, infection, bleeding, and injury to internal organs. In addition, sometimes surgeons are unable to finish the procedure, which is likely devastating to both the parents and their children. There's also an ethical dilemma if there's an "unequal separation." Families also have to consider the following scenarios: whether one will die after separation, whether both will die after separation, or whether they both will die without separation.
One study claims only 60% of surgically separated cases survive, according to the National Center for Biotechnology Information.
Gastric bypass
Some people who want to lose weight and struggle with diet and exercise seek a surgical solution known as gastric bypass. Other people have serious health problems related to their weight, such as gastroesophageal reflux disease, heart disease, Type 2 diabetes, stroke, and cancer. This procedure involves building a small pouch from the stomach and connecting it to the small intestine, according to the Mayo Clinic. After surgery, food enters the small pouch and empties into the small intestine.
Patients may lose 50% or more of their body weight afterwards, according to the University of Iowa Hospitals and Clinics. Rapid weight loss following the surgery can cause the following symptoms within three to six months: body aches, hair thinning or loss, or mood changes. Patients may also feel as though they're sick with the flu. While patients rarely die after surgery, there are some possible complications, including excessive bleeding, infection, blood clots, breathing problems, gastrointestinal system leaks, bowel obstruction, gallstones, hernia, hypoglycemia, ulcers, vomiting, malnutrition, and stomach perforation.
One patient wrote on her blog, My Gastric Bypass Surgery Story, that following the surgery, "The cramping was crazy and came in waves like I was having birth contractions and an alien was gonna climb out." She added, "I felt that I wanna die feeling and was so close to telling my hubby to warm up the truck and take me to the ER. It was HORRIBLE."
Vertebral Osteomyelitis Surgery (Spinal Surgery)
Vertebral osteomyelitis is also known as spinal osteomyelitis or spondylodiskitis, according to the National Center for Biotechnology Information. This type of infection can occur due to spinal trauma, infections in surrounding areas of the spine, or due to bacteria that spreads from the blood to a vertebra, according to the American Association of Neurological Surgeons. Symptoms of an infection can include back pain, fever, chills, weight loss, muscle spasms, painful or difficult urination, weakness or numbness in the arms or legs, and incontinence.
This condition usually occurs among older people, intravenous drug users, those with HIV, or people with organ transplants or cancer. Some dental procedures can also cause spinal infections because bacteria can enter the bloodstream during the surgery and travel to the spine. The most common cause of spinal infections is the bacteria staphylococcus aureus or E. coli.
The surgery to treat this infection can be lengthy, and complications during the procedure can include high blood loss and the need for additional surgeries at the same site. One to 4% of procedures lead to infections. Post-surgical complications can include recurrence of the infection, fractures, paralysis, permanent neurological defects, chronic pain, and disability. Unfortunately, the one- and two-year mortality rates following surgery are 20% and 23%, according to a study in the European Spine Journal.
Coronary Revascularization
People with coronary artery disease have blocked arteries and can require a surgery known as coronary revascularization. The odds of having coronary artery disease are increased due to smoking, high blood pressure, high cholesterol, and having diabetes, insulin resistance, or a sedentary lifestyle. This type of disease is caused by atherosclerosis, which reduces the width of the large arteries as well as the blood supply to vital organs, according to the Missouri Heart Center. A reduced blood supply to the heart can cause chest pain, a heart attack, and even death. Coronary artery disease can be treated with medication and lifestyle changes. Unfortunately, if the arteries are severely blocked, revascularization surgery is necessary. It can involve the implantation of a stent (angioplasty) or bypass surgery.
According to the Cardiology Advisor, complications of coronary revascularization include perioperative myocardial infarction, low cardiac output, cardiac arrhythmias, atrial arrhythmias, and neurologic complications. These neurological issues can include vision problems, problems with attention, memory issues, and peripheral neurologic complications. One of the worst complications is deep sternal wound infections. A patient can also experience renal insufficiency.
Despite these possible post-surgery problems, cardiology revascularization is known to prolong people's lives. Also good news: According to the National Center for Biotechnology Information, only 2%-3% of people who undergo heart bypass surgery die as a result of the procedure.