Creepy (But Good) Ways AI Is Changing The Future Of Medicine
The concept of artificial intelligence (AI) has been a science fiction pillar for decades, but in the 21st century, it has become science fact. IBM defines AI as "technology that enables computers and machines to simulate human learning, comprehension, problem solving, decision making, creativity, and autonomy." Although sci-fi books, films, and TV shows have tried to shed light on what form that mechanical autonomy could take, the reality is a little more humdrum — and a lot more useful.
Since the 1950s, AI systems have evolved from machines that demonstrate human intelligence to deep learning models capable of thinking for themselves, albeit in a limited fashion. Far from plotting the overthrow of humans, AI is supporting and, in some cases, driving incredible leaps in many industries, particularly the field of human health. The use of artificial intelligence (AI) in medicine has its roots in the data digitization of the 1970s. Fast forward to the mid-2020s, and the technology is being integrated into many aspects of healthcare. While the uninitiated may be concerned or even scared about what these breakthroughs could mean, it's worth keeping in mind there's a lot to be excited about.
Wider use of AI technology will lead to greater oversight, as governments and businesses look to keep everyone safe. AI also has the potential to expand quality, personalized healthcare to millions of people who may not have access. Hype aside, here are 12 creepy (but good) ways AI is changing the future of medicine.
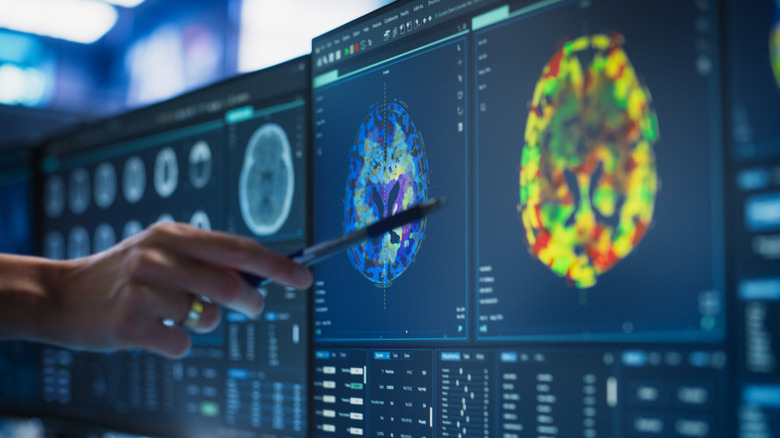
It can analyze medical imaging
One of the most important uses of AI in healthcare is in medical imaging, and although it's still in the earliest phases, the impact has been transformative. Across various experiments, AI has already identified more breast cancers than human clinicians, outperformed dermatologists in skin cancer detection, and been used to read electrocardiograms to spot any potential anomalies. Increasingly sensitive AI technology, applied to X-rays, MRIs, and CT scans, has the potential to support busy doctors and speed up diagnoses without costing a fortune. While the benefits seem obvious, concerns remain about relying on AI for such important decision-making. Some technologies have a low accuracy rate, and not every clinician works well with AI.
In a study led by Harvard Medical School and published in Nature Medicine, researchers found low-scoring radiologists didn't consistently improve with AI support, potentially affecting diagnoses. However, for overworked medics, relying on an AI diagnostic tool could be revolutionary. In 2025, a survey by the UK's Medical Defence Union revealed 69% of doctors suffered from "extreme tiredness," per The Guardian. Support from more sophisticated yet strictly regulated AI technology could enhance diagnostics and allow doctors to do what they do best: Care for patients.
It looks into your medical future
What if we could get a heads-up about chronic disease so it could be spotted and treated earlier? Predictive analytics, backed by artificial intelligence, is making that happen. As the name suggests, data from digital health records is used to predict if we're predisposed to certain conditions. Add genetic and lifestyle information and data from wearables into the equation, and the health picture gets a lot bigger.
Doctors can go from assuming a patient is prone to migraines because of their family history to accurately identifying whether a pregnant woman is at risk for preeclampsia. AI can also assess huge amounts of data to pinpoint patients likely to have complications after surgery and reduce hospital readmissions. In the future, it could also help reduce the risk of rejection among organ donors.
Though AI-backed predictive analytics has a lot of potential, it relies on broad access to our most personal data. Most laypeople also have no idea how deep learning systems work — they don't know how much information they need and what to do with it. Algorithmic bias is another issue: Many programs view race as biological rather than social. However, the New York City Health Department is working to end that practice in an attempt to make predictive analytics and its associated health benefits benefit everyone.
Clinicians can get an AI second opinion
In the United States, it takes around 11 to 15 years just to qualify as a doctor. In the years after that, clinicians accumulate a vast amount of knowledge and insight that they call on to diagnose and treat patients. Traditionally, if they need another pair of eyes on a case, they turn to a colleague, but leaps in technology mean artificial intelligence is increasingly able to offer an informed second opinion.
It's one thing to use the internet to Google a symptom, but trusting AI to back a qualified doctor's diagnosis is another. Yet it could solve a serious problem. A 2024 study found that of 2,428 diagnoses, 17% resulted in "temporary or permanent harm to patients," per JAMA Internal Medicine. For specific illnesses, such as cancer, using AI to interpret the results of complex nuclear scans could be game-changing in countries with huge populations, like India.
Although there is potential for AI to support doctors in their decision-making, it could also hamper the process. At three U.K. stroke centers, it aimed to accelerate diagnosis but instead created "additional verification practices that could paradoxically slow the diagnostic process," via Nature. More creepy is what could happen in the future if artificial intelligence is seen as a diagnostic authority: Would AI creators have more clout than an experienced doctor?
Voice technology that does more than take notes
Millions of people own smart technology with female voice assistants that respond to their every spoken command, and growing numbers are using voice search to find or buy things on the internet. But it's not just commerce that's reaping the benefits — voice and AI are combining to form what could be a powerful tool in the world of medicine. Scientists at the University of South Florida are training AI models to listen to people's voices and detect signs of illness, identifying biomarkers for Parkinson's disease, diabetes, and mental health issues, as well as the onset of menopause. And though research is ongoing, using AI to assess someone's voice could also provide a non-invasive, cost-effective way to predict whether someone is likely to develop Alzheimer's disease.
While AI could potentially help many people using just their voices, experts have raised an important point: It could identify information that a patient wants to keep private. AI can already differentiate between smokers and non-smokers with up to 72% accuracy, according to the Luxembourg Institute of Health's Colive Voice research program. Technology that knows more than what people reveal to their clinicians could harm the doctor-patient relationship and even impact treatment.
Finding new drugs, faster
It took eight months to develop the first COVID-19 vaccine, but medical experts and scientific researchers usually spend years looking for and developing new drugs. Artificial intelligence is speeding up that process, while at the same time exploring treatment avenues that might be considered off-the-wall or strange (remember, some modern-day drugs used to be used as cough medicine). But is it a bit creepy to allow technology to be creative or insightful when it comes to making new drugs?
Programs like Google DeepMind's AlphaFold helped revolutionize our knowledge of protein structures, but there's still room for improvement in the predictions that AI makes from data sources. Even if sophisticated systems aren't 100% accurate when assessing the likelihood of how novel compounds behave, some scientists say allowing them to push the envelope under controlled conditions is a good idea. Genentech is spearheading a "lab in a loop," in which data is used to predict drugs and treatments. These projections are tested within the same laboratory ecosystem, reducing research and development time and honing the AI model's performance. According to Harvard Medical School's Marinka Zitnik, the tech could even use experimental results to generate treatments that have positive real-world effects or focus on conditions that have flown under the research radar.
Personalized medicine at the genetic level
In 2003, scientists finished the mammoth task of mapping the human genome, and ever since, researchers have been using its insights to further the field of personalized medicine. Forget simply knowing about your family history and which lifestyle choices could impact your health. This is healthcare at the genetic level, and artificial intelligence could make it more targeted than ever.
Doctors who know the genetic predispositions of their patients can tailor treatments so they're more accurate and effective, with few or even no side effects. But current medicine is still some way from that goal, as IBM Watson's genomic initiative demonstrated. It set out to identify personalized treatments for patients but failed due to "poor data quality, inadequate clinical validation, and unrealistic timelines," per Henrico Dolfing.
Another clinical area where genetics has proved helpful is maternity screening, which can help parents prepare for inherited diseases or conditions in their children. AI is being used to spot any subtle changes or chromosomal abnormalities, allowing time for specific plans and even personalized treatments to be put in place. While some might think it strange for generations of babies to be genetically profiled before birth, being able to create and match medication to their unique DNA could be the future of healthcare.
Monitoring patients remotely, 24/7
Technology, including AI, has been used in public surveillance and data gathering for years: Think CCTV, facial recognition software, and even your car spying on you. In healthcare, it's playing an increasingly important role in the remote monitoring of patients. AI-enabled sensors keeping an eye on someone's breathing, heart rate, or temperature can quickly flag up any sudden changes, and that real-time personal data feed can enhance the treatment of illness.
There are other ways seniors or people with long-term or chronic conditions stand to benefit from advances in AI monitoring technology. Smart systems can issue timely reminders for patients to take their medication, ensuring they stick to their personalized treatment plans. For the elderly or isolated, they can also provide much-needed companionship. Remote monitoring using AI-backed technology can also help clinicians predict patient behavior, potentially avoiding hospitalization or additional medication.
Filling our homes with devices that are watching and listening to us may help keep us healthy, but there's a "Big Brother" element that is a little creepy to some. Questions are already being asked about how much personal data people will be happy to hand over and the sorts of incentives companies could offer for them to do so. If the payoff is a healthier, happier population thanks to targeted treatments and informed clinicians, it might be worth it.
Virtual health assistants worth talking to
Millions of businesses use chatbots to interact with their customers, and the healthcare industry is no different. Virtual assistants ask simple questions and use the inputted replies to suggest solutions — from drinking more water to seeking emergency care — or schedule a doctor's appointment. Although there have been instances where human-AI chatbot interactions have gone awry, AI-backed virtual health assistants are going much further.
Nurses are responsible for a lot of patient support, like answering questions about doctors or treatments or sending information to clinicians. Virtual nursing assistants that have been trained on vast amounts of medical data are already helping to lift this burden. While some may feel uneasy about sharing personal health information with an app or a bot rather than discussing their issues with a human, a Syneos Health Communications report found that most patients have no problem.
AI-backed virtual nursing assistants are more sophisticated than ever, providing personalized, human-like responses that are designed to put worried people at ease. For patients and nurses, they are a win because they shift the human contact to where it is needed most: during treatment. Being able to access information about treatments or symptoms at any time — and in multiple languages — provides real-time, informed patient support and leaves real-world nurses free to focus on bigger issues.
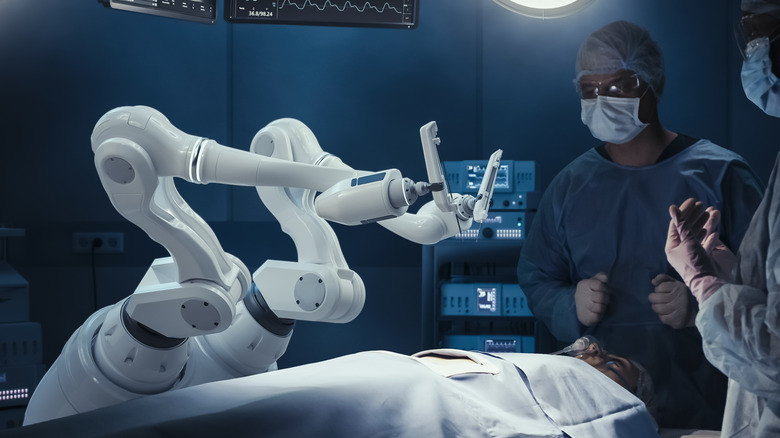
Taking robotic surgery to the next level
Humans have used robots for longer than you might think, but in 1985, a brain biopsy operation broke new ground for being the first procedure to use a surgical robot. In the 21st century, they are used across multiple procedures around the world. The technology has become so advanced, surgeons can manipulate the robots with total accuracy from thousands of miles away. Artificial intelligence has an important role to play in ensuring these complex surgeries are successful.
AI can ensure that surgical implants are accurately positioned, create 3D models of preoperative CT scans, and merge CT and MRI data to boost the accuracy of a robot's or surgeon's movements. In 2024, a surgeon in Germany used AI-enhanced goggles to visualize a tumor in its entirety as part of his preparation, enabling him to see important blood vessels before an incision was made.
Artificial intelligence is proving useful outside the operating theater too. In 2025, an Annals of Surgery study used the technology to scan patient selfies to assess if their surgical incisions were infected. It is also increasingly being used in medical education and training, in line with the rise of virtual and augmented reality bodies in the place of real human cadavers. Although the use of AI-backed robotics can enhance training and, for surgical patients, reduce hospitalization times, concerns remain. There are no clear answers about who would be accountable for a mechanical error, even as technological advances "seek to expand the capabilities of surgical robots," per the Journal of Robotic Surgery.
Prioritizing patients over paperwork
From the moment we're born, medical staff are recording information that tells them everything about us, and it's a workload all its own. Clinicians spend almost as much time on patients' electronic health records as they do on physical care. But that is changing, thanks to digital technology and artificial intelligence.
Note-taking is a labor-intensive but vital part of healthcare, and growing numbers of companies have developed AI-based solutions to automate this task. As well as freeing up a lot of doctors' time, these digital systems can also keep better track of patient data and make it easier to share information between clinicians. AI is even helping to maximize operating theaters, providing a more efficient workflow than paper systems. Who said AI was only good for dusty, ancient texts?
Anything that gives doctors more time for patients has to be a good thing, but relying on AI so heavily has given some cause for concern. In 2024, OpenAI's transcription tool Whisper was reported as having "hallucinations," or making up comments. If a "hallucination" happens or a mistranscription occurs, it could have catastrophic implications. Even creepier, some people might not even be aware that their doctor is using AI to take notes. But with appropriate levels of transparency and reliable, robust systems, doctors and patients could see real benefits.
AI everywhere: From the ambulance to the operating theatre
When ambulance crews respond to an accident, every second counts, and information gathered at the front line can impact what happens to patients in the emergency room and operating theater. EMS vehicles carry an array of technology to save people's lives, but AI is helping get crews to emergency situations faster. Combining AI with traffic monitoring and GPS systems enables dispatchers to get EMS crews' locations efficiently and safely. Many bigger towns and cities have smart, internet-of-things systems that connect with ambulances, enabling them to effectively clear a path to the location where they're needed. AI has also proved to be groundbreaking for paramedic training, bringing it a long way from its groundbreaking origins. It has enabled teams to learn about complex injuries and treatments outside a pressured accident scenario.
While there are risks in increasing the role of AI in frontline healthcare, with hospitals becoming targets for hackers, the technology has a lot of potential. Researchers at Sweden's Chalmers University of Technology found that AI models outperformed their human counterparts in assessing the level of injuries in patients. According to researcher Anna Bakidou, their hope is that AI can be regarded as an "extra colleague" and "makes staff see more complex connections and think twice in cases where injuries can be difficult to perceive or assess," via Healthcare in Europe.
More screening for everyone?
Many people wear smart gadgets that monitor their heart rate, blood oxygen levels, or breathing to keep an eye on various aspects of their health. Medical researchers want to harness AI and these non-invasive technologies via smartphones to screen entire communities. The aim is to identify people with potential health issues and ensure they get treatment.
Because so many of us have smartphones, they're a ready-made tool for a wide range of screening applications. AI-backed algorithms can use cellphone images to identify skin disease (though not as well as dogs can detect cancer) or assess hemoglobin levels, while the device's microphones could be used to screen people for lung or neurological diseases. As well as large-scale use, AI screening can help individual patients too: A tool developed by the National Institutes of Health helped cut readmissions among adults at risk for opioid use, and the tech could help identify teenagers at risk of mental health issues.
Researchers in the British Journal of General Practice said of AI in screening: "As these systems become better validated, they will be given more responsibility." While the medical community is in favor of technology that improves access to healthcare for all, ethical concerns surrounding "social disparities, creating power imbalances, and locking in oppressive systems" continue to be discussed (via BMJ Health & Care Informatics).