The Messed Up History Of Polio
Although polio is thought to have been around for thousands of years, it didn't reach pandemic proportions until the 20th century. And while it's highly contagious, a vast majority of polio cases are asymptomatic, which made it difficult to track transmission and isolate those who were infected.
In roughly 2 percent of cases, polio is so severe that it affects the muscles and causes paralysis in the limbs... and the muscles needed for breathing. The difficulty breathing that people with polio suffered from is what led to the invention of the iron lung, which confined thousands of young children and is still used by some in 2020.
The eradication of wild polio has been one of the more successful medical campaigns that science has undertaken. As of 2020, two out of the three types of wild polio have been eradicated in every country except for Afghanistan and Pakistan. However, there are still cases of vaccine-derived polio and until wild polio is completely wiped out, there remains a risk of a worldwide resurgence, so it's good to be aware just how bad it used to be. This is the messed up history of polio.
Causes and symptoms of polio
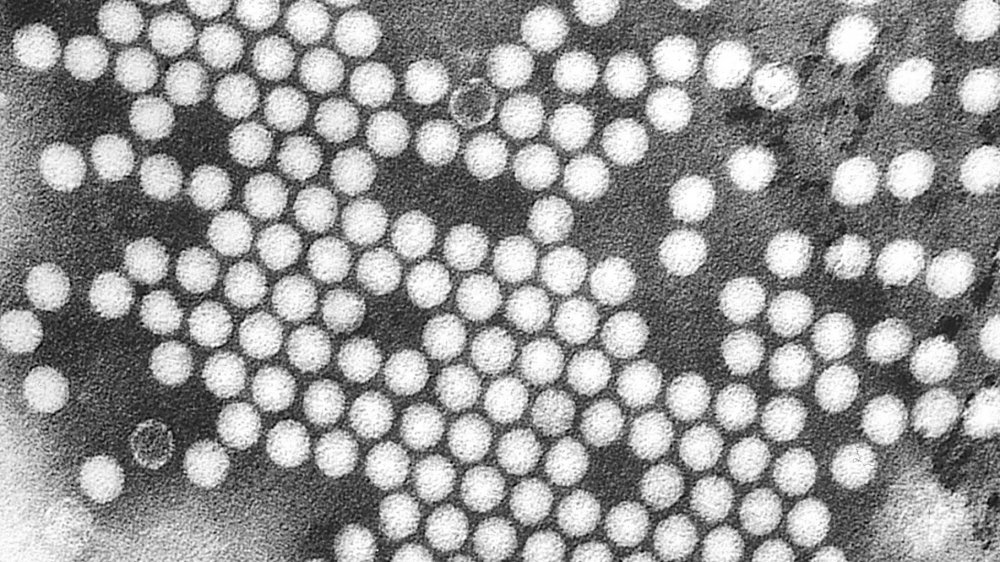
Polio, also known as poliomyelitis, is caused by the poliovirus. According to the CDC, there are three types of wild polioviruses, Types 1, 2, and 3. However, Type 2 and Type 3 were declared to have been eradicated in 2019. Polio is considered to be a highly contagious disease, although it can only be spread amongst humans. According to the European Centre for Disease Prevention and Control, the poliovirus spreads through aerosols or droplets and enters through the mouth during person-to-person contact, or via fecal contamination of water, utensils, food, or hands.
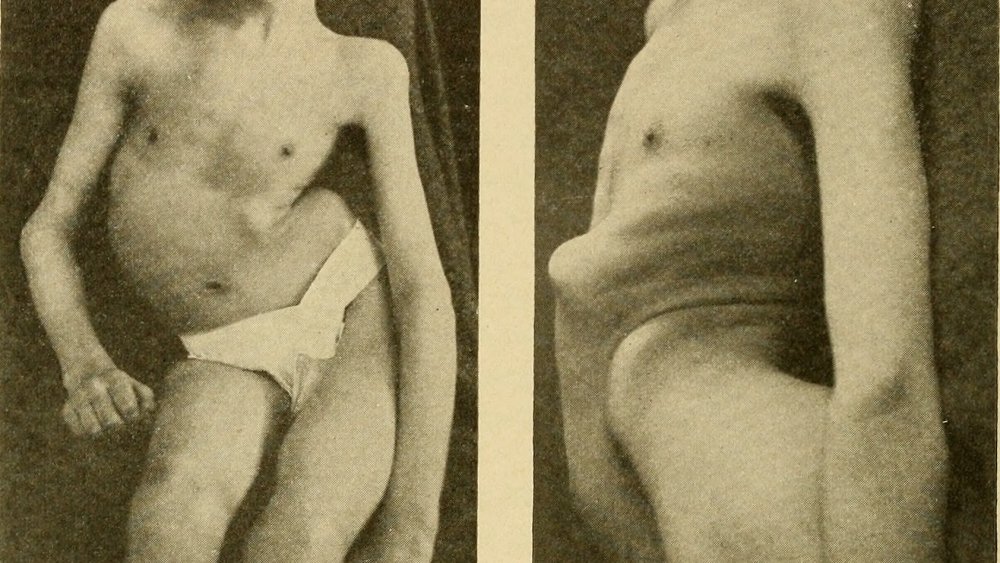
Although as much as 95 percent of polio infections are asymptomatic, people are infectious even without displaying symptoms. Symptoms of a polio infection can include fever, vomiting, back and neck pain, and muscle weakness. Referred to as nonparalytic polio, this type of polio infection can last up to 10 days and most people are able to recover completely. There also exists a milder form, known as abortive polio, where symptoms are so mild that they may be mistaken for the flu. These types of polio account for around 4-8 percent of infections.
However, up to 2 percent of polio cases result in paralytic polio, which results in paralysis in the brainstem, spinal cord, or both. According to the WHO, among those with paralytic polio 5-10 percent die as a result of immobilized breathing muscles.
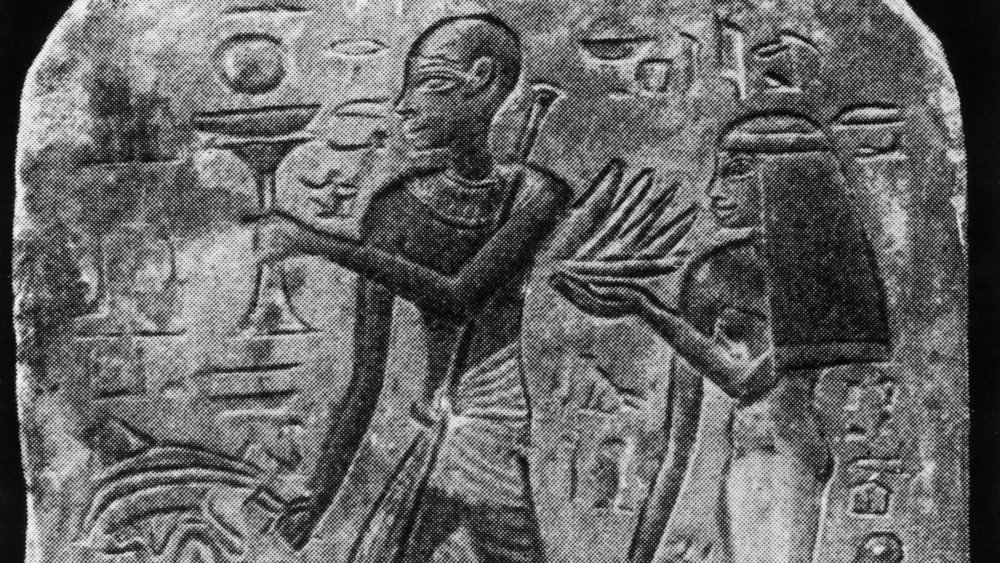
Polio has been around for thousands of years
Although polio didn't reach its epidemic rates until the 1800s, there's evidence that polio has been around for thousands of years. The mummy of the pharaoh Siptah, who ruled from 1197 to 1191 BC, bears a deformity of the left foot and leg that is suggestive of polio or cerebral palsy. And according to the BBC, an Ancient Egyptian stone carving, also known as a stele, which dates from 1404-1365 BC depicts a priest with a walking stick and one leg thinner than the other, also characteristic of polio.
An Attic pelike vase from 5th century Ancient Greece similarly depicts a person with thinner lower limbs and a spinal deformity, using the aid of a walking stick. However, descriptions of polio-like illnesses are few and far between and it's not so easy to distinguish visual representations from other diseases. And since polio infections appeared sporadically, with infrequent cases of acute paralytic polio, the first recognizable description of polio doesn't appear until the 18th century.
The first clinical description of polio
In the late 18th century, pediatrician Michael Underwood gave the first discernible medical description of polio. In 1789, Underwood identified an illness afflicting children in a medical textbook, describing it as "debility of the lower extremities which gradually become more infirm, and after a few weeks are unable to support the body."
According to the National Museum of American History, it would take another 50 years for orthopedist Jacob von Heine to describe polio involvement and effect on the spinal column. Heine distinguished the disease from other types of paralysis and named the disease "infantile spinal paralysis." And according to the Journal of Neurology, Neurosurgery and Psychiatry, the pathology of polio wasn't identified until 1855 when several doctors identified the atrophy that occurs in the spinal gray matter. Wilhelm Heinrich Erb kept this in mind when he named the disease "acute anterior poliomyelitis" in 1875, combining the Greek terms for gray (polio) and marrow (muelos) to reflect an inflammation of spinal gray matter.
Unfortunately, according to Biographies of Disease: Polio, none of these physicians recognized the incredibly contagious nature of polio or foresaw the epidemics to come.
The first polio epidemics
While there were sporadic clusters of polio across Europe in the early 1800s, the first epidemic occurred in 1868, when there were at least 14 cases near Oslo, Norway. Then, in 1881, there were at least 13 cases in northern Sweden. In 1894, the state of Vermont was hit hard, with 132 people left with permanent paralysis and 18 deaths. And according to the Washington Post, most of the victims of the Vermont polio outbreak were between 5- and 10-years-old.
The polio outbreak in Vermont is the first well-documented polio epidemic. Unfortunately, doctors still didn't believe that the disease was contagious. According to the History of Vaccines, Charles Caverly, a doctor who wrote on the paralytic epidemic in Vermont, claimed that "it is very certain that it was non-contagious."
But because doctors weren't necessarily required to report polio diagnoses to the public health authorities, it's difficult to track how widespread polio epidemics were until it became a reportable disease in the early 1900s. According to Polio, the next largest outbreak occurred in New York in 1907, with over 1,000 recognizable cases of polio. Since epidemics of polio were increasing in severity, frequency, and size, it's possible that the virus was evolving during these early epidemics.
The 1916 polio epidemic
In the summer of 1916, New York was struck with a particularly severe polio epidemic. According to the Washington Post, upwards of 9,000 cases were reported. Nationwide, there were over 27,000 cases. Unfortunately, the figures don't distinguish between paralytic and non-paralytic cases. According to The Conversation, public health authorities attempted to contain the epidemic and cut lines of transmission through isolation and treatment, but they were unaware of the infectious nature of asymptomatic cases. As a result, the medical certificates that deemed people free of symptoms were next to useless. Pools and movie theaters were closed, but polio often spread amongst households, especially amongst those who didn't have a private toilet.
Because polio was first diagnosed in two children from the Italian community in Brooklyn, Italian immigrants were blamed for the epidemic and at times physically assaulted, despite the fact that their own infection rates were actually low. Many people were also afraid that their pets were spreading polio and on July 26, 1916, the SPCA in New York City reported that they'd collected and killed 80,000 pets from fearful owners.
According to The Open Microbiology Journal, doctors tried a variety of methods, ranging from intraspinal injections to nasal sprays. Adrenaline was given both intramuscularly and intraspinally, but over 50 percent of people who received this treatment died. Unfortunately, despite the fact that the epidemics were soon overshadowed by WWI and the influenza epidemic of 1918, polio didn't subside.
Annual summer epidemics
Polio continued to wreak havoc in communities across the United States, and even future-president Franklin D. Roosevelt contracted polio in 1921 and was left permanently paralyzed from the waist down as a result. During the 1940s and 1950s, the United States suffered from annual polio epidemics during the summer and early fall which were so severe that summer became a fearful time and many children were confined to their homes. Since the transmission of polio was still not entirely understood, indoor public gathering places were closed and doctors recommended staying away from swimming places. According to the Minnesota Department of Health, Minnesota's State Fair was cancelled in 1946 in order to reduce the transmission of polio.
There was also a desire amongst physicians to subdue what they referred to as "an epidemic of hysteria" and many questioned whether or not the number of polio deaths should even be released. Doctors such as Robert Barr also wondered what other information people might start to demand, claiming that "accidental deaths will be the next one they will be wanting to know."
According to The Conversation, by 1953 polio was polled to be the second most frightening thing for Americans, right after "nuclear annihilation."
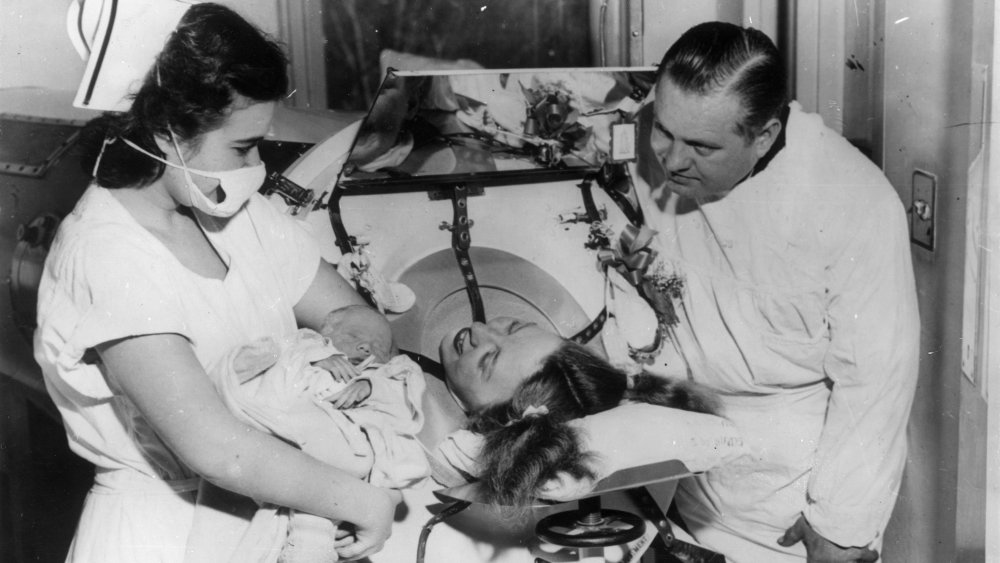
The iron lung
Iron lungs operate by applying negative pressure, which allows a person with polio to breathe. The pressure causes a person's chest muscles and diaphragm to mimic the movement of breathing, forcing air out the mouth as pressure increases and drawing air in as pressure decreases.
According to Polio Voices: An Oral History from the American Polio Epidemics and Worldwide Eradication Efforts, the iron lung was invented by Philip Drinker in 1928, having experimented first on cats and later his colleagues. The machine was significantly improved by John Emerson a few years later. The first person with polio to try an iron lung was an 8-year-old girl, and she was sustained by the machine for five days until she succumbed to an unrelated infection. The iron lung went from prototype to clinical use in a very short amount of time with little-to-no testing for efficacy or safety. And although at first iron lungs were used only in emergency situations, physicians soon became comfortable using them as the number of machines and patients increased.
However, few considered the ethical implications of condemning someone to spending their life in an iron lung. While some people only required iron lung treatment for several weeks or months, depending on the severity of paralysis some people would require the iron lung for the rest of their lives. Rocking beds were developed in the late 1940s to help wean some people off iron lungs. The movement of the mattress helped pull and push air in and out of the lungs, although they were ultimately less effective than iron lungs.
Koprowski's active viral vaccine
Inspired by Max Theiler's development of a yellow fever vaccine, Hilary Koprowski set out to create a polio vaccine in the late 1940s. Koprowski's vaccine was made from an active virus, compared to an inactive virus vaccine, which uses formaldehyde to destroy the virus's ability to produce disease while maintaining virus particles. Koprowski used the same method of attenuation as Theiler, moving the poliovirus through the brains of rats to reduce its virulence until the virus weakened but was still able to provoke an immune response. Koprowski tested the vaccine on chimpanzees and himself, and then proceeded to move onto human trials. Unfortunately, his test subjects consisted of 20 mentally disabled children in Letchworth Village in Rockland County, New York. Thankfully, none of them developed complications.
Despite the unfortunate fact that experimentation on mentally disabled children was commonplace at the time, when Koprowski reported his results in 1951, many researchers were rightfully horrified. According to Cambridge Medical History, in the mid-1930s, two scientists in the United States, Maurice Brodie and John Kolmer, had tested polio vaccines on children with tragic results. Brodie's vaccine, made with an inactive virus, didn't induce enough antibodies, and sometimes caused allergic reactions, while Kolmer's virus, also made with a live virus, hadn't been properly attenuated and as a result caused several cases of polio.
Although Koprowski's vaccine was eventually successfully used on four continents around the world, the United States never approved it for use.
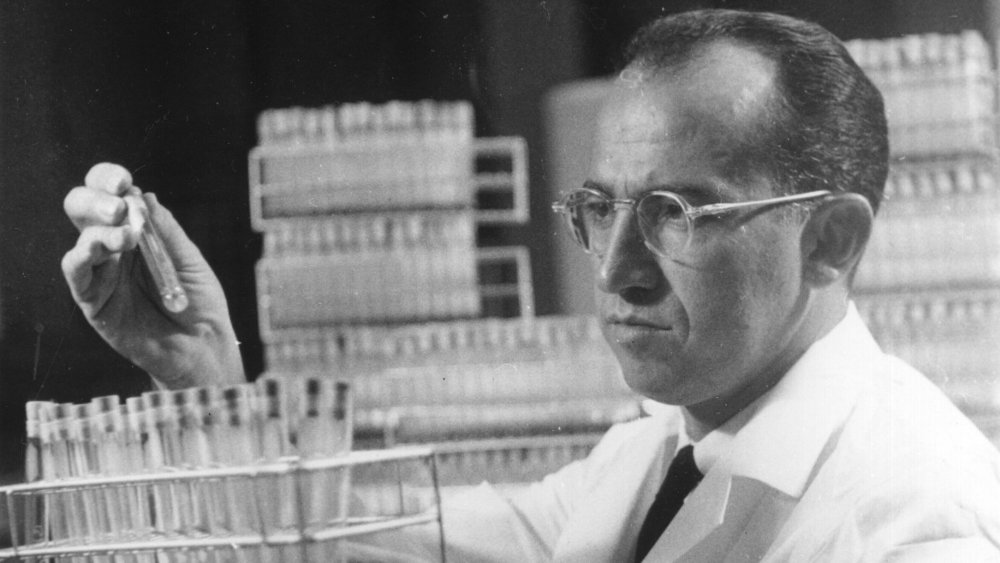
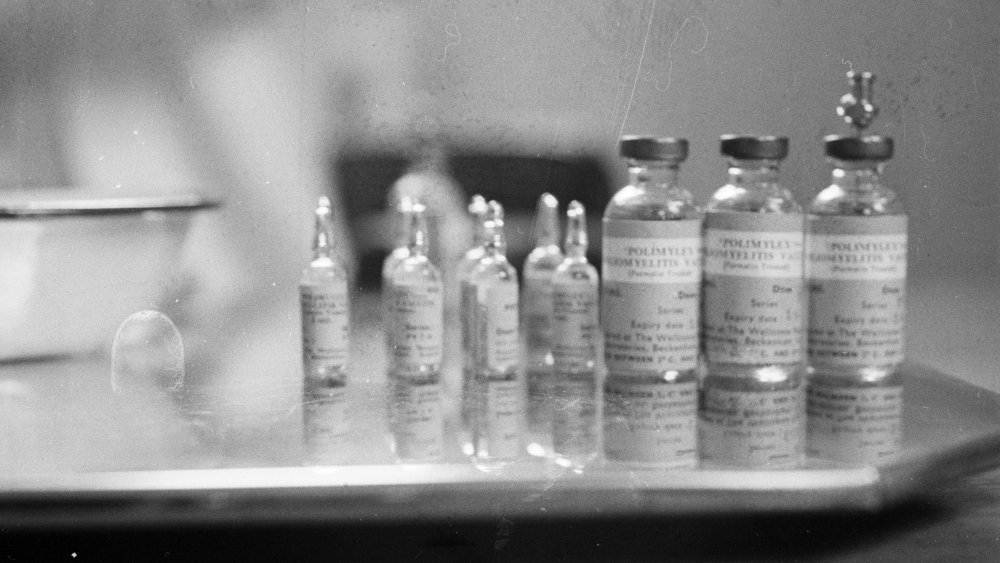
Salk's inactive viral vaccine
In the 1950s, Jonas Salk also made a polio vaccine, although his was made out of an inactive dead virus compared to Koprowski's active (though non-virulent) virus. (While Salk gets all the credit, a number of women, like Elise Ward, were also pivotal to the work done on his vaccine.) According to The Conversation, after Salk demonstrated the viability of his vaccine on laboratory monkeys and two small groups of children with and without polio, the National Foundation for Infantile Paralysis sponsored one of the largest field trials in medical history.
According to American Heritage, the trial began on April 26th, 1954, and took a year to analyze the results and determine if the vaccine was safe and effective. Administered via injection, over 600,000 children were given either a placebo or the Salk vaccine while over one million other children were monitored as a control group.
Although President Dwight D. Eisenhower said that the polio vaccine should be available to every child, he didn't say how that was going to happen, appointing Health, Education and Welfare Secretary Oveta Culp Hobby to figure it out. Meanwhile, Hobby herself claimed that free vaccines would open the "'back door' to socialized medicine." Hobby also said that the production of the vaccine should be done by private companies so although Salk didn't patent his vaccine, price gouging by private companies resulted in the price of the vaccine soaring from $2 to $20.
The difference between the Salk and Sabin vaccines
Around the same time as Salk was working on his vaccine, Albert Sabin was also working on a vaccine, using the same live-virus technique that Koprowski had used. According to Science History Institute, after developing three strains of poliovirus that appeared to induce antibodies without causing paralysis, Sabin tested his oral vaccine on himself, his research associates, and his family. Sabin also tested his polio vaccine on people who were imprisoned at Chillicothe Penitentiary. Although, according to the University of Cincinnati, people volunteered for experimentation, it's unclear how ethically sound Sabin's experiments were.
By this point, Salk's vaccine was already being used in the United States and Sabin was unable to get funding for a large-scale trial like Salk's. But in 1957, Sabin convinced the Soviet Union to conduct a trial with his vaccine. After the trial was deemed a success in 1960, the United States approved Sabin's vaccine in 1961 for manufacture.
Although Sabin's vaccine was easier to administer and less expensive, there was still a one in 750,000 chance of contracting polio from the attenuated live virus. Thus, in order to finally eradicate polio Salk's vaccine needed to be made widely available around the world.
The Cutter incident
Salk's vaccine was dealt a vicious blow when in April 1955, one of the laboratories manufacturing the vaccine didn't successfully inactivate the virus, resulting in 40,000 outbreaks of polio. Known as The Cutter Incident, the United States Department of Health, Education and Welfare determined the defective vaccines stemmed from the California-based Cutter Laboratories.
According to The Conversation, Cutter Labs had failed to follow Salk's detailed instructions on how to properly kill the virus and make the vaccine. As a result, children were essentially just being injected with the poliovirus itself. 200 children who developed polio as a result of the improperly prepared vaccine ended up with varying degrees of paralysis and 10 children lost their lives to polio.
In response, the government instituted a committee of scientists to screen the polio vaccine and by mid-June inoculations resumed under stricter government oversight. Congress also passed the Polio Vaccine Assistance Act of 1955 to allow for a wider public dispersion of the vaccine. Unfortunately, the damage was already done and many were fearful and uncertain of the efficacy of the vaccine.
Contamination of SV40
In 1960, it was discovered that almost 30 percent of polio vaccines were contaminated with Simian Virus 40, or SV40, a virus that's known to increase the risk of cancer. According to Oncogene, this likely occurred because the vaccines had been created in monkey kidney cell cultures that had harbored SV40.
After it was discovered, the contamination was eliminated from future vaccines, but since SV40 is similar to other cancer-causing viruses, there was a fear that the contamination might've resulted in increased rates of cancer. But according to Immunization Safety Review, researchers have been unable to conclusively establish if SV40 causes cancer in humans, and there's still no evidence to suggest that people who got the polio vaccine between 1955 and 1963 have an increased rate of cancer.
Plus what likely occurred, according to Vaccination: A History from Lady Montagu to Genetic Engineering, is that while killing the poliovirus with inactivating agents such as formaldehyde and beta-Propiolactone, the SV40 virus ended up inactivated as well.
Polio in the world today
In the world, Type 1 wild polio remains endemic in Afghanistan and Pakistan, while it's considered to have been eradicated in the rest of the world. However, instances of vaccine-induced polio still continue to occur throughout the world, due to the use of an active oral vaccine rather than the inactive injection vaccine.
The United States eradicated wild polio by 1979, and compared to 1988, polio cases worldwide have decreased by 99 percent. According to NPR, the African continent was declared to be free of wild polio in 2020 after four years since the last reported case of wild polio.
But despite the almost complete eradication of wild polio, many countries still suffer from vaccine-derived cases since the vaccine they receive is with a weakened, but alive, form of the poliovirus that is able to mutate and spread in under-immunized communities. Between August 2019 and August 2020, upwards of 20 countries around the world reported instances of vaccine-derived polio.